Cofactor AI: Revolutionizing Insurance Denial Appeals
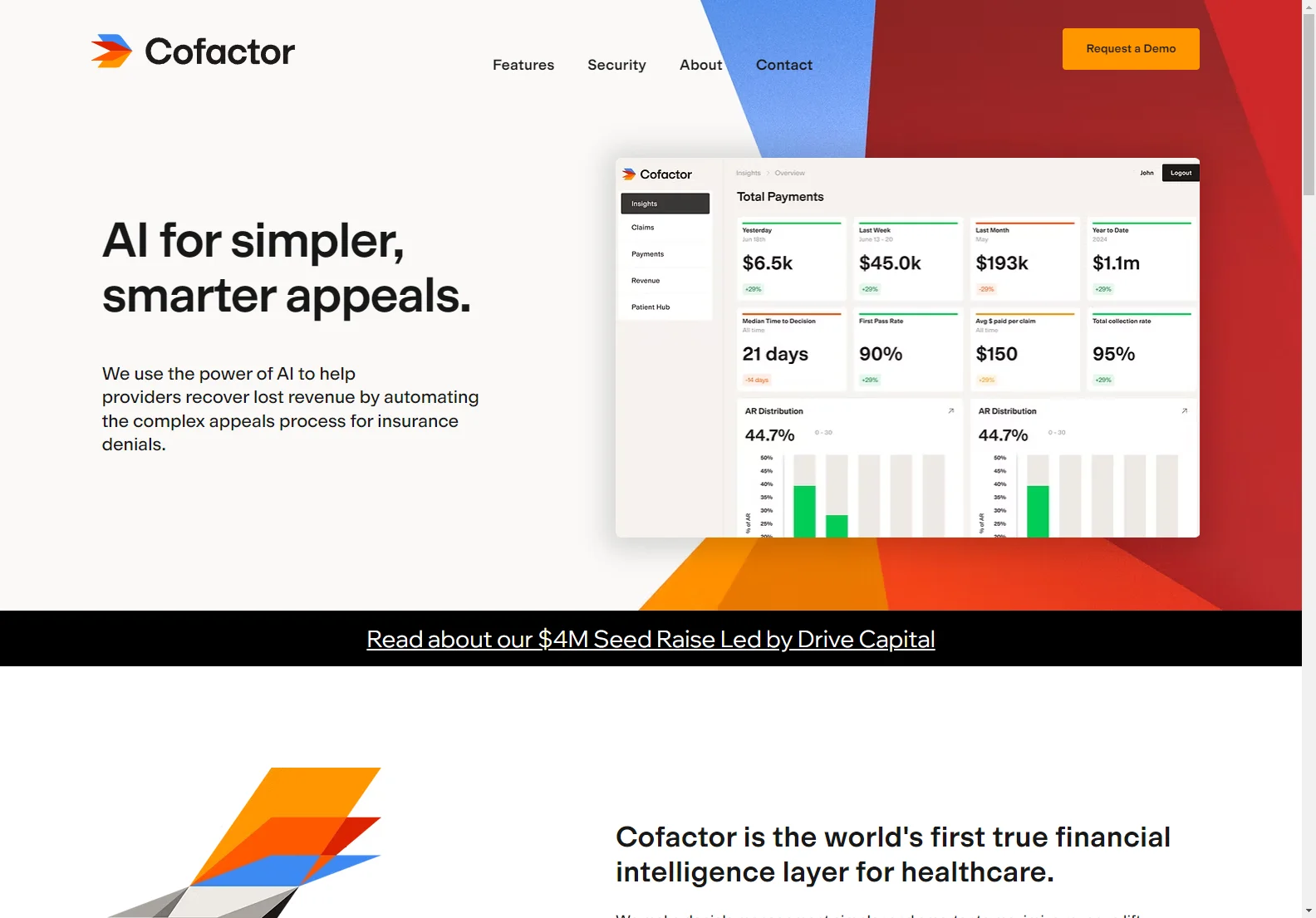
Cofactor AI is a game-changer in the world of healthcare and insurance. It utilizes the power of AI to automate the complex appeals process for insurance denials, helping providers recover lost revenue.
In the 'Overview' section, it's clear that Cofactor AI simplifies and streamlines the appeals process. It identifies root causes of denials, prioritizes claims, and automates complex appeals in seconds, maximizing revenue recovery.
The 'Core Features' of Cofactor AI are impressive. It increases overturn rates by leveraging AI-powered insights to identify exactly what evidence payers need. It also improves appeal efficiency by automating documentation gathering, submission formatting, and status tracking across all payers. Additionally, it recovers more revenue per year by catching every appealable denial and maximizing success rates. It reduces the cost to collect by transforming the appeals process into a streamlined, automated workflow. Finally, it reduces days outstanding, transforming the revenue cycle with automated appeals.
In the 'Basic Usage' section, users can streamline their appeals process with Cofactor AI and maximize their revenue recovery. The platform is secure and trusted, with a dedicated compliance team ensuring the highest standards of data security through regular audits and security reviews.
Overall, Cofactor AI is a powerful tool that is changing the landscape of insurance denial management and helping healthcare providers improve their financial outcomes.